Understanding the success rates of Clomid, HCG, and IUI can help you make informed decisions about fertility treatments. Research indicates that the combination of Clomid and HCG injections can improve ovulation rates significantly. Specifically, studies show that approximately 60-80% of women taking Clomid experience ovulation, and those who also receive HCG may see an increase in the chances of successful conception.
In terms of intrauterine insemination (IUI), success rates vary widely based on several factors, including age, underlying fertility issues, and timing of the procedure. Generally, the success rate for IUI when combined with Clomid can range from 10% to 20% per cycle. Women under 35 typically experience higher success rates compared to older age groups.
For maximizing chances of success, it’s advisable to schedule the IUI procedure soon after the HCG injection, as this timing closely aligns with ovulation. Regular monitoring through ultrasounds can also assist in determining the optimal time for the procedure. Consulting with a fertility specialist to tailor a treatment plan based on individual circumstances can further enhance the likelihood of achieving pregnancy.
- Clomid, HCG, and IUI Success Rates: A Comprehensive Overview
- Understanding the Mechanism: How Clomid and HCG Work Together in IUI
- Coordinating Treatment Protocols
- Managing Side Effects and Expectations
- Statistical Success Rates: What to Expect from Clomid and HCG in IUI Procedures
- Factors Influencing Success Rates
- Combination Approach Benefits
- Factors Influencing Success: Key Elements That Impact Clomid HCG IUI Outcomes
Clomid, HCG, and IUI Success Rates: A Comprehensive Overview
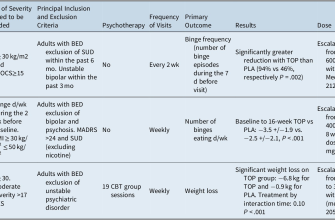
Clomid and HCG significantly influence the success rates of intrauterine insemination (IUI). Studies indicate that using Clomid can enhance ovulation, resulting in an increase in the chances of conception during IUI cycles. The typical success rate for IUI when combined with Clomid ranges between 10% to 20% per cycle.
Administering HCG serves as a trigger for ovulation, and its timing is crucial. Successful ovulation usually occurs about 36 hours after HCG is given. Aligning the timing of IUI with ovulation can lead to improved success rates. Many clinics recommend performing IUI 24 to 36 hours post-HCG injection, maximizing the potential for sperm to meet the egg.
Factors such as age, fertility diagnosis, and motility of sperm also play a role in outcomes. Women under 35 often report higher success rates, around 15% to 20% per cycle. In contrast, rates decline with advancing age, particularly beyond 40, where success rates may drop to less than 5% per cycle.
Combining Clomid and HCG with IUI presents a strategic approach for couples facing infertility challenges. Monitoring the response to Clomid through ultrasounds helps tailor the treatment, ensuring optimal timing for the insemination procedure. Adjustments to dosage based on individual response can also enhance effectiveness.
In conclusion, collaborating with a fertility specialist ensures a personalized plan that takes into account specific medical histories and goals, improving overall success rates. Regular assessments and ongoing support contribute to a more successful treatment experience.
Understanding the Mechanism: How Clomid and HCG Work Together in IUI
Clomid and HCG synergistically enhance fertility outcomes during intrauterine insemination (IUI). Clomid, an oral medication, stimulates the ovaries to produce multiple eggs by blocking estrogen receptors in the hypothalamus. This blocking leads to increased secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), driving ovarian follicle development.
Once you achieve optimal follicle growth with Clomid, HCG plays a pivotal role. Administered as an injection, HCG mimics the natural LH surge that signals the ovaries to release mature eggs. This timing is critical, as it prepares the eggs for fertilization during IUI. Following HCG administration, scheduling the IUI procedure within 24 to 36 hours maximizes the chances of successful conception.
Coordinating Treatment Protocols
Healthcare providers typically recommend Clomid cycles of 5 days, starting on the third to fifth day of your menstrual cycle. Monitoring through ultrasounds allows for assessing follicle size and determining the right moment for HCG injection. Proper synchronization of these medications optimizes follicle health and increases the likelihood of sperm meeting egg.
Managing Side Effects and Expectations
Patients may encounter side effects from Clomid, such as mood swings or ovarian hyperstimulation. Discuss these with your healthcare provider to manage discomfort effectively. Understanding this process empowers you to maintain realistic expectations regarding IUI success rates, which can be influenced by age, fertility diagnosis, and previous treatments.
Statistical Success Rates: What to Expect from Clomid and HCG in IUI Procedures
Clomid combined with HCG for intrauterine insemination (IUI) shows promising success rates, particularly for women under 35. The average success rate in this demographic ranges from 15% to 20% per cycle. These rates improve significantly when multiple cycles are considered, with about 50-60% of couples achieving pregnancy after three to six IUI attempts.
Factors Influencing Success Rates
Success rates can vary based on several factors. Age plays a crucial role; women over 35 typically experience lower success rates, around 10% to 15% per cycle. Additionally, the underlying cause of infertility affects outcomes. For instance, unexplained infertility may yield higher success rates with Clomid and HCG compared to other specific conditions such as severe male factor infertility. Monitoring follicle development via ultrasound enhances timing and increases the likelihood of success.
Combination Approach Benefits
Using Clomid for ovarian stimulation followed by HCG to trigger ovulation optimizes the chances of conception. The combination helps produce multiple mature follicles, thus maximizing sperm exposure during the insemination process. Many clinics recommend this approach, leading to a more favorable success rate compared to IUI without stimulation. Tracking hormonal levels also helps in tailoring the treatment for better results, resulting in a more personalized and effective approach to IUI.
Factors Influencing Success: Key Elements That Impact Clomid HCG IUI Outcomes
Age significantly affects Clomid, HCG, and IUI success rates. Women under 35 typically experience higher pregnancy rates compared to those over 35. Hormonal balance plays a critical role; irregular cycles may lower success rates.
Egg quality directly correlates with fertility treatments. Higher quality eggs enhance the likelihood of implantation and pregnancy. Regular monitoring of follicle development through ultrasounds allows for better timing of IUI procedures.
Male sperm quality also influences outcomes. Factors like sperm count, motility, and morphology contribute to the success of fertilization. It’s advisable for male partners to undergo a semen analysis prior to treatment.
Health and lifestyle choices greatly impact results. Maintaining a balanced diet, regular exercise, and avoiding smoking or excessive alcohol enhances fertility. Weight management, particularly avoiding obesity, improves hormonal balance and increases chances of conception.
Timing of the IUI procedure is vital. Conception is most likely when the IUI is performed within 24 hours of ovulation. Triggering ovulation with HCG ensures that this timing aligns perfectly with egg release.
- Pre-existing medical conditions: Conditions like endometriosis or polycystic ovary syndrome (PCOS) can hinder success rates.
- Previous pregnancy history: A positive pregnancy history increases the likelihood of success with subsequent treatments.
- Psychological wellbeing: Stress management techniques may improve outcomes. Consider counseling or support groups.
Regular follow-ups with a fertility specialist ensure that any necessary adjustments to the treatment plan are made promptly. This adaptive approach maximizes the chances of success by tailoring the process to individual needs and responses.