A growing body of evidence supports the use of Naltrexone in treating binge eating disorder (BED). Research indicates that this medication can reduce the frequency of binge eating episodes and help individuals regain control over their eating habits. Naltrexone functions by targeting the brain’s opioid receptors, which play a significant role in reward processing and impulse control.
Patients often report a decrease in cravings and a heightened ability to resist the urge to binge. Clinical studies have shown promising results, with many participants experiencing significant reductions in binge eating days per week. Combining Naltrexone with therapy, such as cognitive-behavioral therapy, enhances the overall effectiveness of the treatment program.
It’s important to consult with a healthcare provider to determine the appropriate dosage and monitor for potential side effects. As with any medication, individual responses can vary. Alongside pharmacological treatment, developing healthy coping mechanisms and addressing emotional triggers are essential for long-term recovery and well-being.
- Naltrexone and Binge Eating Disorder: An In-Depth Exploration
- Mechanism of Action
- Clinical Evidence and Recommendations
- Understanding Binge Eating Disorder and Its Symptoms
- The Role of Naltrexone in Treating Binge Eating Disorder
- Mechanism of Action: How Naltrexone Affects Eating Behaviors
- Comparative Effectiveness: Naltrexone vs. Traditional Treatments
- Clinical Evidence: Studies Supporting Naltrexone Use for Binge Eating
- Key Studies and Findings
- Mechanism of Action
- Potential Side Effects and Considerations When Using Naltrexone
- Guidelines for Prescribing Naltrexone for Binge Eating Disorder
- Initial Dosing
- Monitoring and Follow-Up
- Patient Experiences and Outcomes on Naltrexone Therapy
- Reported Improvements
- Side Effects and Management
Naltrexone and Binge Eating Disorder: An In-Depth Exploration
Naltrexone shows promise in addressing Binge Eating Disorder (BED) by reducing the frequency of binge episodes and curbing cravings. This medication, primarily used for opioid dependence, works by blocking opioid receptors in the brain, which helps to diminish the reinforcing effects of food and decrease the urge to binge eat.
Mechanism of Action
By inhibiting the opioid receptors, Naltrexone alters the brain’s reward pathway associated with eating. Binge eating often correlates with emotional disturbances and cravings. Naltrexone helps manage these emotional triggers by stabilizing mood and lowering the impulse to seek out food for comfort.
Clinical Evidence and Recommendations
Clinical studies reveal that Naltrexone reduces binge eating frequency. In trials, participants reported fewer binge episodes and improved control over their eating habits. When combined with behavioral therapies, the results are often more significant. It’s advisable for individuals considering Naltrexone treatment to discuss potential benefits and side effects with a healthcare provider, as individual responses can vary.
Maintaining a balanced diet and engaging in regular physical activity can enhance the effectiveness of Naltrexone. Monitoring progress and any side effects closely ensures the regimen remains appropriate for managing Binge Eating Disorder effectively. Support groups or therapy can provide additional strategies and encouragement during treatment.
Understanding Binge Eating Disorder and Its Symptoms
Binge Eating Disorder (BED) involves recurring episodes of consuming large quantities of food in a short period, often accompanied by feelings of loss of control. Individuals with BED may eat even when they’re not hungry and continue eating until they feel uncomfortable.
Common symptoms of BED include eating incredibly fast, eating in secret, and feeling distressed regarding eating habits. After binge episodes, guilt or shame frequently arises, impacting emotional well-being. This disorder varies from other eating disorders as it does not typically involve purging behaviors.
Pay attention to behavioral signs such as frequent fluctuations in weight, withdrawal from social activities centered around food, and dietary restrictions followed by episodes of uncontrolled eating. Individuals might create rituals around food, such as eating alone or hiding food in unusual places.
Recognizing these symptoms can facilitate early intervention. Encouraging those affected to seek professional help can lead to better coping strategies and a healthier relationship with food. Professional treatments often combine therapy and, in some cases, medications like naltrexone, which can help reduce cravings.
The Role of Naltrexone in Treating Binge Eating Disorder
Naltrexone has shown promise in treating binge eating disorder by targeting underlying neurobiological mechanisms. This medication operates primarily as an opioid receptor antagonist, which helps to modulate the brain’s reward pathways associated with food intake. By reducing the reinforcing effects of binge eating, naltrexone can diminish the frequency and severity of episodes.
Clinical studies indicate that naltrexone may lead to a significant decrease in binge eating days per week. Patients often experience reduced cravings and enhanced impulse control, enabling them to make healthier choices. Moreover, naltrexone is typically well-tolerated, with manageable side effects, making it a suitable option for many individuals seeking assistance with this disorder.
For optimal outcomes, combining naltrexone with cognitive behavioral therapy enhances treatment effectiveness. This dual approach addresses not just the physiological aspects of binge eating, but also the behavioral and emotional triggers that contribute to the disorder. Patients report improved self-monitoring skills and emotional regulation, fostering long-term adherence to healthier eating patterns.
Individuals considering naltrexone should engage in a thorough discussion with their healthcare provider. Personal medical history and co-occurring conditions can influence the suitability and dosage of the medication. Regular follow-up appointments ensure that any necessary adjustments are made promptly, maximizing the potential benefits of treatment.
Naltrexone demonstrates a valuable role in the multifaceted treatment landscape for binge eating disorder. By enabling individuals to regain control over their eating behaviors, it helps pave the way toward a healthier future.
Mechanism of Action: How Naltrexone Affects Eating Behaviors
Naltrexone works by blocking opioid receptors in the brain, influencing the reward system associated with eating. This reduces cravings often linked to binge eating episodes.
Naltrexone also modulates dopamine pathways, which play a crucial role in the reinforcement of behaviors. By altering dopamine levels, it can decrease the reinforcing effects of food, shifting the focus away from food as a primary reward.
Additionally, the medication impacts the hypothalamus, an area of the brain that regulates hunger and satiety signals. By balancing these signals, naltrexone helps regulate appetite, reducing the instances of overeating.
Research indicates that combining naltrexone with other treatments, such as psychotherapy, enhances the overall management of binge eating disorder. This comprehensive approach addresses both psychological triggers and physiological responses, promoting sustainable change in eating behaviors.
Regular monitoring and adjustments to treatment can optimize the effectiveness of naltrexone in combating binge eating episodes. Consulting with a healthcare provider ensures the appropriate dosage and support throughout the process.
Comparative Effectiveness: Naltrexone vs. Traditional Treatments
Naltrexone shows promise as a treatment for binge eating disorder, often producing better outcomes than traditional approaches such as cognitive behavioral therapy (CBT) or standard dietary changes. Clinical trials indicate that individuals using Naltrexone report fewer binge episodes compared to those solely relying on psychotherapy.
One study demonstrated that participants on Naltrexone experienced a significant reduction in binge frequency, with an average decrease of around 50% over 12 weeks, while CBT alone resulted in a reduction of about 30%. These findings highlight Naltrexone’s ability to address the underlying neurobiological mechanisms associated with binge eating.
Combining Naltrexone with psychotherapy can yield superior results. Patients receiving both therapies often experience greater satisfaction and adherence to the treatment regimen. This dual approach allows for addressing both the psychological aspects of eating behavior and the pharmacological inhibition of cravings.
Safety profiles differ as well. Naltrexone generally has a favorable safety record, with side effects such as nausea or fatigue being mild and manageable. In contrast, traditional treatments may carry risks related to dependency or other psychological side effects. Monitoring patients on Naltrexone has led to minimal complications, emphasizing its suitability as a long-term option.
Ultimately, individuals struggling with binge eating disorder may find that Naltrexone provides a compelling alternative or complement to traditional treatments. Those considering this medication should discuss it with healthcare providers to tailor the approach to their specific needs.
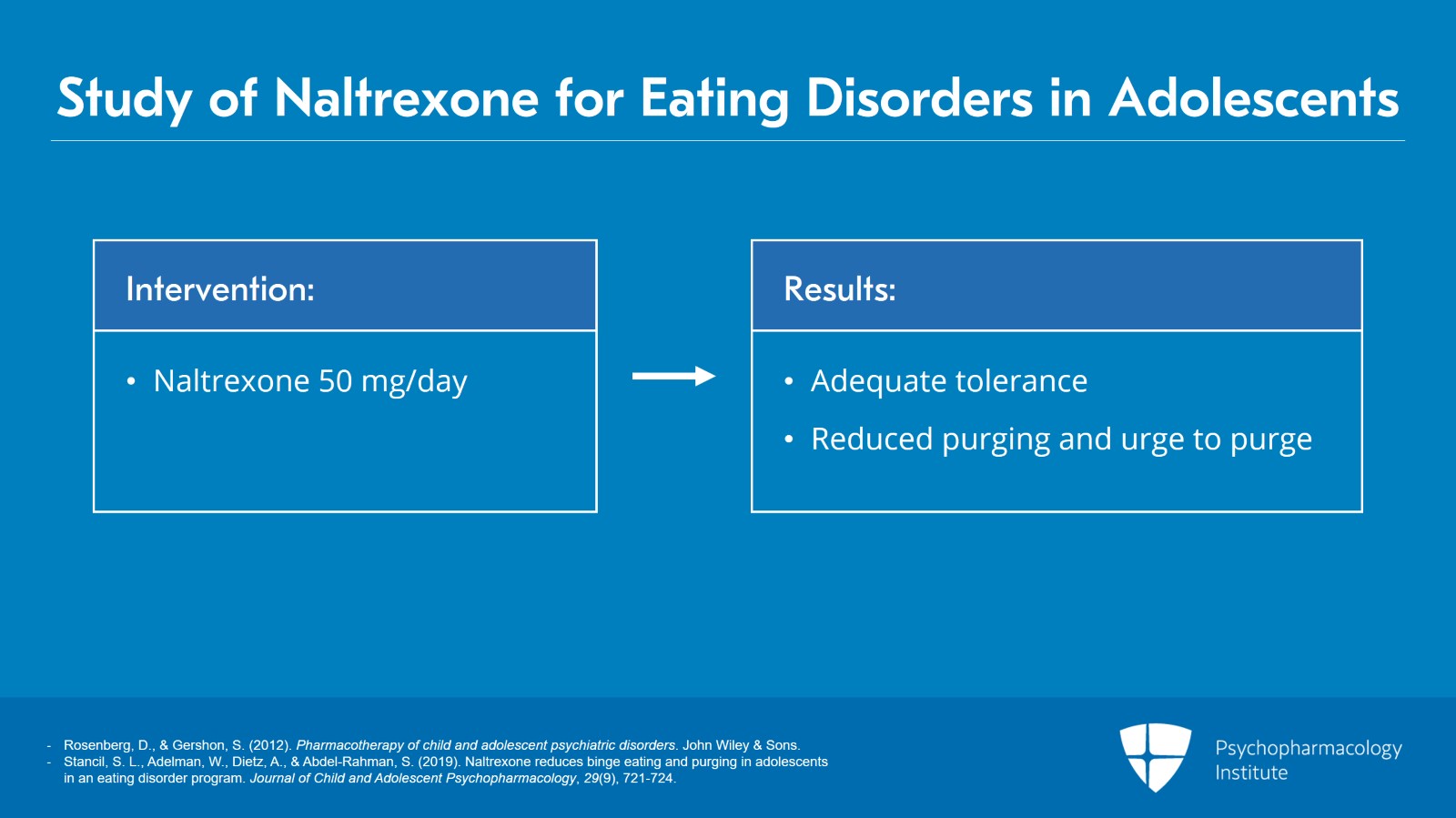
Clinical Evidence: Studies Supporting Naltrexone Use for Binge Eating
Research demonstrates that naltrexone provides significant benefits for individuals with binge eating disorder (BED). Various clinical trials have supported its efficacy in reducing binge eating episodes and associated symptoms.
Key Studies and Findings
-
Trial by D. A. G. et al. (2013): This randomized controlled trial showed that participants receiving naltrexone experienced a marked decrease in binge eating frequency compared to the placebo group. By the end of the 12-week study, 50% of those on naltrexone reported fewer than one binge episode per week.
-
Research from McElroy et al. (2000): This study highlighted the drug’s ability to improve food craving control. Participants noted a reduction in cravings, which correlated with reduced binge eating incidents, suggesting naltrexone affects the brain’s reward pathways.
-
Long-term Effects (Wilfley et al., 2017): Analysis over a 24-week period indicated sustained weight loss in participants treated with naltrexone. The study emphasized the importance of combining pharmacotherapy with counseling for optimal outcomes.
Mechanism of Action
Naltrexone operates as an opioid receptor antagonist. By blocking opioid receptors, it decreases the reward from binge eating behavior, leading to a declining cycle of binge and compensatory behaviors. Patients reported not only fewer binges but also an overall improvement in emotional well-being.
Continued investigation into naltrexone reveals its promise as a frontline treatment for BED. With consistent findings from diverse studies, clinicians now consider naltrexone a favorable option for managing this complex disorder.
Potential Side Effects and Considerations When Using Naltrexone
Monitor for common side effects such as nausea, headache, dizziness, and fatigue. Chills and sleep disturbances may also occur. Those sensitive to medication should start with a lower dose to assess tolerance.
Be aware of the risk of liver damage. Regular liver function tests are necessary, particularly for individuals who consume alcohol or have pre-existing liver conditions. Avoid alcohol during treatment, as it can amplify side effects and strain the liver.
Interactions with other medications can impact treatment. Share your complete medical history with your healthcare provider, including any prescription or over-the-counter drugs. This will help identify potential interactions.
Psychological effects might manifest, such as mood swings or increased anxiety. If these symptoms arise, consult a healthcare professional promptly. Adjustments in dosage or alternative treatments may be necessary.
Compliance requires consideration of the requirement for opioid-free status before initiating Naltrexone. Taking opiates can lead to withdrawal symptoms, emphasizing the importance of adherence to guidelines.
For those with a history of substance use disorder, ongoing support from a therapist or support group could enhance treatment success. Regular follow-ups with healthcare providers are recommended to monitor overall progress and address any emerging side effects or concerns.
Guidelines for Prescribing Naltrexone for Binge Eating Disorder
Assess the patient’s history and current condition before initiating naltrexone therapy. Confirm a diagnosis of binge eating disorder (BED) using standardized criteria. Evaluate any coexisting medical or psychiatric conditions that may influence treatment.
Initial Dosing
Start with a low dose, typically 25 mg once daily. Monitor the patient for any adverse effects, especially within the first week. Gradually increase the dose every three to four days based on tolerance and clinical response, up to a maximum of 100 mg daily. Adjustments should account for individual patient factors.
Monitoring and Follow-Up
Schedule regular follow-up appointments, at least every four weeks, to evaluate the effectiveness of treatment and monitor for side effects. Use validated scales to measure binge eating frequency and associated behaviors. Maintain open communication to address any concerns the patient may have regarding side effects or treatment progress.
- Consider laboratory tests to monitor liver function, as naltrexone can impact liver health.
- Discuss the importance of lifestyle modifications, including diet and physical activity.
- Encourage participation in behavioral therapy alongside medication for a more holistic approach.
Be attentive to the possibility of opioid use and contraindications. Naltrexone is not suitable for patients currently using opioids or those who have not completed a detoxification program. Educate the patient about potential withdrawal symptoms if opioid use is abrupt.
Evaluate the continuity of care. If treatment is effective, consider long-term maintenance therapy while regularly assessing the need for ongoing support. Adjust the strategy as needed based on the patient’s evolving needs and feedback.
Patient Experiences and Outcomes on Naltrexone Therapy
Naltrexone therapy has shown promising results for patients with binge eating disorder (BED). Many individuals report significant decreases in binge eating episodes after starting treatment. A common observation is the improved ability to regulate cravings, leading to more stable eating patterns.
Reported Improvements
Patients frequently share that their emotional relationship with food evolves positively. They describe a reduction in the compulsive need to eat and a growing sense of control over their choices. Many participants in clinical studies point out decreased urges, which allows them to participate in social events without feeling overwhelmed by food-related anxiety.
Side Effects and Management
While most users tolerate naltrexone well, some experience mild side effects such as nausea or headaches. Understanding these potential reactions helps set realistic expectations. Most side effects subside within a few weeks as the body adjusts to the medication. Regular communication with healthcare providers ensures timely management of any discomfort, encouraging better adherence to therapy.
| Patient Feedback | Outcome |
|---|---|
| Reduced binge eating frequency | Improved overall well-being |
| Increased feelings of fullness | Less emotional eating |
| Better control over cravings | Enhanced quality of life |
| Improved social interactions | Less food-related anxiety |
Patients often express gratitude for regaining a sense of normalcy with their eating habits. The support network, including healthcare professionals and family, plays a crucial role in reinforcing their commitment to treatment. Regular check-ins promote accountability and help sustain motivation through the recovery process.