If you suspect an allergy to penicillin or clindamycin, consult your healthcare provider for proper testing and alternative treatment options. Allergic reactions can range from mild rashes to severe anaphylaxis, making immediate assessment crucial. To ensure safety, patients with known allergies should always inform their doctors before receiving any medication.
Penicillin allergy occurs in approximately 10% of the population, but many individuals incorrectly believe they are allergic after experiencing mild side effects. Cross-reactivity with other antibiotics, like amoxicillin, can occur. In cases of penicillin allergy, clindamycin often serves as a suitable alternative, particularly for infections where penicillin is indicated.
However, it’s important to recognize that clindamycin itself can also cause allergic reactions, albeit less frequently. Symptoms may manifest as skin rashes, itching, or gastrointestinal disturbances. A history of hypersensitivity reactions to one antibiotic requires careful evaluation before the use of another. Always discuss your complete medical history with your healthcare provider to prevent adverse effects.
Understanding Penicillin and Clindamycin Allergy
Patients with a documented allergy to penicillin should exercise caution when prescribed clindamycin, as there may be overlapping side effects, although the risk of cross-reactivity is low. Clindamycin is a lincosamide antibiotic primarily used for treating bacterial infections.
Recognizing symptoms of an allergic reaction is critical. These can include:
- Rash or hives
- Itching
- Swelling of the face, lips, or tongue
- Difficulty breathing or wheezing
When experiencing any of these symptoms after taking either antibiotic, seek medical attention immediately.
Before starting clindamycin, inform your healthcare provider about your history of allergies, including reactions to penicillin. Conduct thorough discussions regarding alternative antibiotics if necessary.
An allergy test may be recommended for those unclear about their sensitivities. Skin testing can provide insights into potential reactions and guide appropriate treatment options.
For those with a confirmed penicillin allergy, clindamycin often serves as a suitable alternative for treating infections like strep throat, certain skin infections, and dental procedures.
Monitor closely for any signs of allergic reactions upon initiating clindamycin. Make sure to maintain open communication with your healthcare provider about any concerns related to medications.
In conclusion, understanding your allergies and discussing any concerns with your physician will streamline your treatment plan and enhance your safety.
Identifying Symptoms of Penicillin Allergy
If you suspect a penicillin allergy, monitor for specific symptoms. Common manifestations include:
Skin Reactions: Hives, rashes, or itching may appear shortly after taking the medication. These reactions often present as redness or swelling.
Respiratory Issues: Difficulty breathing, wheezing, or anaphylaxis is serious. Seek immediate medical attention if you encounter these symptoms.
Gastrointestinal Distress: Nausea, vomiting, or diarrhea can occur. Pay attention to any significant changes after antibiotic intake.
Swelling: Noticeable swelling of the face, lips, or throat calls for urgent care. These symptoms could indicate angioedema.
Keep a detailed record of any reactions experienced after taking penicillin. Consult your healthcare provider for evaluation and potential allergy testing. This proactive approach helps ensure safe medical care in the future.
Cross-Reactivity Between Penicillin and Clindamycin
Penicillin and clindamycin belong to different classes of antibiotics, which significantly reduces the likelihood of cross-reactivity. Penicillin, part of the beta-lactam group, can trigger allergic reactions such as rashes, hives, or anaphylaxis. Clindamycin, an lincosamide, does not share the same chemical structure, making it safer for individuals with penicillin allergies.
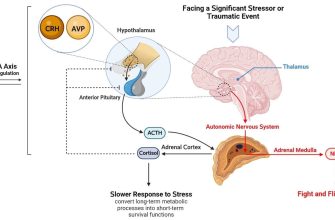
Understanding Allergic Reactions
Allergic reactions to antibiotics often arise from the immune system identifying a specific molecule as a threat. Since clindamycin lacks the beta-lactam ring present in penicillin, most patients with penicillin allergies can safely use clindamycin. However, a small percentage of patients may still experience adverse effects, necessitating medical supervision prior to administration.
Guidelines for Use
Healthcare providers should assess the patient’s allergy history carefully. In patients with a confirmed penicillin allergy, clindamycin serves as a recommended alternative for treating infections, particularly in cases involving staphylococci or anaerobic bacteria. Conducting a skin test for clindamycin may offer additional reassurance for those with a history of severe antibiotic allergies.
Management Strategies for Allergic Reactions
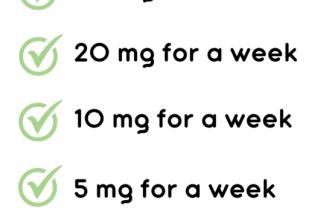
Immediately identify and discontinue any medication causing an allergic reaction. In mild cases, administering an antihistamine can alleviate symptoms such as rash or itching. For moderate to severe allergic reactions, including anaphylaxis, carry epinephrine auto-injectors and administer them as prescribed. Always ensure the affected individual has access to emergency medical services.
Monitor vital signs closely following an allergic incident. If symptoms such as difficulty breathing, swelling, or rapid heartbeat occur, seek emergency help right away. Provide a calm environment as stress can exacerbate symptoms.
Document the specific allergic reaction details for future reference. Include the drug involved, reaction severity, and response to treatment. Share this information with healthcare providers, ensuring they adjust future prescriptions accordingly.
Consider consulting an allergist for skin testing or blood tests to determine specific drug sensitivities. This professional assessment provides clarity on safe medication alternatives. Encourage open communication with healthcare providers regarding any past allergies, and always carry an allergy alert card to inform emergency personnel.
Educate the patient and their family about recognizing symptoms of allergic reactions to ensure timely action. Training on the use of epinephrine and knowledge of local emergency procedures enhances safety and readiness.