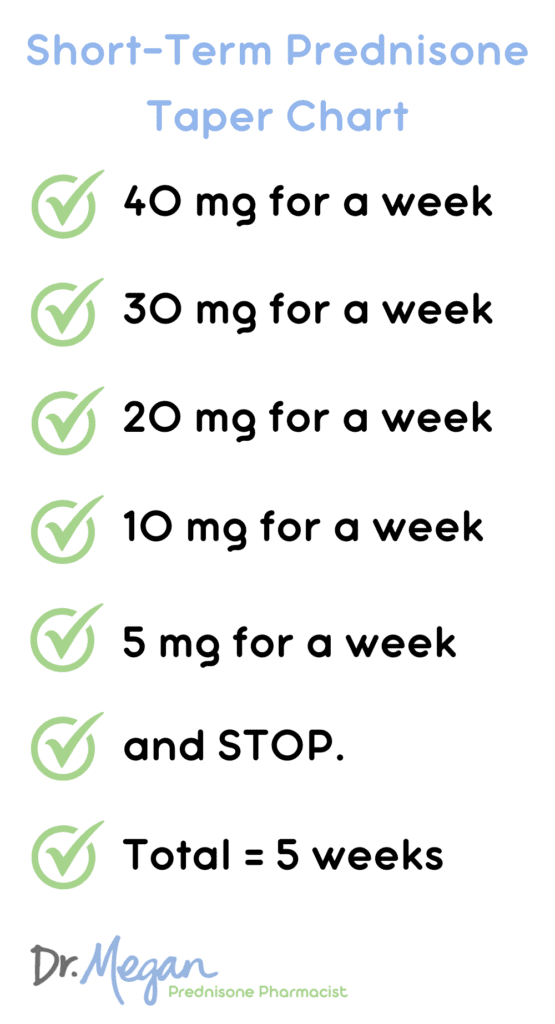
Begin the tapering process of prednisone at 40 mg with a gradual reduction schedule tailored to your individual needs. Reducing the dosage too quickly can lead to unwanted withdrawal symptoms, including fatigue, joint pain, and a flare-up of underlying conditions. Aim to decrease the dosage by 5 mg increments every week or as directed by your healthcare provider.
Monitor your response closely during the tapering period. Document any changes in your symptoms, energy levels, or side effects to share with your doctor. Adjustments might be necessary based on how your body reacts. Keeping an open line of communication with your healthcare team helps ensure a smoother transition.
As you approach lower dosages, consider incorporating lifestyle changes that support your overall health. Adequate hydration, balanced nutrition, and gentle physical activity can help mitigate the effects of tapering. Always follow your provider’s advice, as they can offer personalized recommendations to enhance your tapering experience and promote recovery.
- Prednisone 40 mg Tapering Dosage Guide
- Sample Tapering Schedule
- Monitoring and Adjustments
- Understanding Prednisone and Its Uses
- Common Uses of Prednisone
- Dosage and Administration Tips
- Initial Dosing: Starting with 40 mg
- Titration and Monitoring
- Considerations for Special Populations
- How to Create a Tapering Schedule
- Establish a Reduction Plan
- Monitor Symptoms
- Managing Withdrawal Symptoms During Tapering
- Hydration and Nutrition
- Supportive Therapies
Prednisone 40 mg Tapering Dosage Guide
Begin tapering from 40 mg by reducing the dose gradually to minimize withdrawal symptoms and prevent flare-ups of the underlying condition. A common approach is to decrease the dose by 5 mg every week. For example, start with 35 mg for one week, then 30 mg for the next week, and continue this pattern until reaching a lower maintenance dose or discontinuation.
Sample Tapering Schedule
Here’s a sample schedule for tapering from 40 mg:
- Week 1: 40 mg
- Week 2: 35 mg
- Week 3: 30 mg
- Week 4: 25 mg
- Week 5: 20 mg
- Week 6: 15 mg
- Week 7: 10 mg
- Week 8: 5 mg
- Week 9: Discontinue or adjust as advised by a healthcare provider
Monitoring and Adjustments
Regularly monitor your symptoms during tapering. If symptoms worsen, consult a healthcare professional. Adjustments to the tapering schedule may be necessary based on individual response and underlying health issues. Always communicate any side effects or concerns with your doctor for tailored guidance.
Understanding Prednisone and Its Uses
Prednisone is a corticosteroid that reduces inflammation and suppresses the immune system. It treats a variety of conditions, including asthma, autoimmune diseases, and allergic reactions. Proper use is essential for managing symptoms effectively.
Common Uses of Prednisone
- Asthma and chronic obstructive pulmonary disease (COPD) management.
- Treatment of autoimmune disorders such as lupus and rheumatoid arthritis.
- Management of severe allergic reactions and skin conditions.
- Reduction of inflammation in conditions like colitis or dermatitis.
Dosage and Administration Tips
Start with the recommended dosage, typically 40 mg for specific acute conditions. Gradually taper the dosage to minimize withdrawal symptoms. Monitor for side effects such as mood changes, weight gain, or increased blood pressure.
- Consult a healthcare provider for individualized dosing.
- Follow a tapering schedule to avoid abrupt discontinuation.
- Keep track of symptoms and report any concerning changes to your doctor.
Prednisone can interact with other medications. Discuss all prescriptions and over-the-counter drugs with a healthcare professional. This ensures safe and effective treatment while minimizing potential complications.
Initial Dosing: Starting with 40 mg
Begin treatment with a prednisone dosage of 40 mg daily. This dosage suits various conditions, including autoimmune disorders and severe allergies. Administer the medication in the morning to mimic natural cortisol production. Consistency in timing helps maintain stable levels in the body.
Titration and Monitoring
After initiating therapy, assess the patient’s response at regular intervals. Monitor for both effectiveness and side effects, such as increased appetite or mood changes. Adjust the dosage based on clinical response while considering the patient’s specific needs and health status.
Considerations for Special Populations
For elderly patients or those with comorbid conditions, evaluate the risk of complications. Start at a lower dose if necessary and gradually increase. Patients with pre-existing conditions like diabetes or hypertension may require additional monitoring. Tailor the tapering process to ensure safety and minimize adverse effects.
How to Create a Tapering Schedule
To create an effective tapering schedule for prednisone 40 mg, begin by consulting your healthcare provider for personalized guidance. They can help determine the best starting point for your dose reduction based on your specific health needs.
Establish a Reduction Plan
Implement a gradual tapering plan, reducing your dose by 5 mg every week. This approach helps minimize withdrawal symptoms and allows your body to adjust. Adjust the tapering rate based on your response; if necessary, slow down the reduction process.
Monitor Symptoms
Keep a journal to track any symptoms or side effects during the tapering process. Note changes in mood, energy levels, and any physical reactions. This information will be valuable for discussions with your healthcare provider, allowing for adjustments to your schedule as needed.
Stay in regular contact with your doctor throughout the tapering process. Share your observations, and don’t hesitate to report any concerns. They are your best resource for ensuring a safe and effective taper.
Maintaining a balanced diet and practicing stress-reducing techniques, such as mindfulness or gentle exercise, can support your body during this transition. Prioritize adequate hydration and rest to bolster overall well-being.
Managing Withdrawal Symptoms During Tapering
To ease withdrawal symptoms during the prednisone taper, gradually reduce the dosage. Avoid abrupt stops to minimize side effects. Monitor your body’s reactions closely. Maintain a daily journal to track any changes, symptoms, or side effects you experience throughout the tapering process.
Hydration and Nutrition
Stay well-hydrated. Drink plenty of water and consider electrolyte-rich beverages to combat fatigue and muscle cramps. Nutritional support plays a key role; incorporate a balanced diet rich in fruits, vegetables, lean proteins, and whole grains to strengthen your body’s defenses.
Supportive Therapies
Engage in supportive therapies such as gentle yoga or meditation to alleviate stress and improve mood. Regular, light exercise can enhance blood circulation and elevate your overall sense of well-being. Consult your healthcare provider for possible alternatives and additional resources to assist in managing withdrawal symptoms effectively.