For individuals seeking relief from menopause symptoms, Premarin offers a hormone replacement therapy option. This prescription medication primarily contains estrogen and is effective in alleviating hot flashes, vaginal dryness, and other related discomforts. Before considering Premarin, consult with a healthcare provider to determine if this treatment aligns with your health profile and needs.
Understanding the benefits and potential side effects of Premarin is crucial. Many users report significant improvement in their quality of life, experiencing reduced symptoms that accompany hormonal changes. Common side effects may include nausea, headaches, and breast tenderness. Monitoring your body’s response during treatment is advisable, especially in the initial stages of use.
Staying informed about dosage and administration is essential for optimal results. Typically, Premarin is taken once daily, and it’s important to follow your physician’s instructions regarding timing and any dietary considerations. For those with a history of hormone-sensitive conditions, discussing risks and alternatives is vital in making an educated decision.
Regular follow-ups with your healthcare provider will enhance the monitoring of your progress and allow for timely adjustments to your treatment plan if necessary. Emphasizing open communication about any concerns or side effects can greatly contribute to the success of using Premarin in managing menopause symptoms.
- Premarin Prescription: A Comprehensive Guide
- Understanding Premarin: What It Is and How It Works
- Indications for Prescribing Premarin in Hormone Therapy
- Dosage Guidelines for Effective Use of Premarin
- Potential Side Effects and Risks Associated with Premarin
- Important Drug Interactions to Consider with Premarin
- Anticoagulants and Antiplatelet Drugs
- Anticonvulsants and Barbiturates
- Patient Monitoring and Follow-Up During Premarin Therapy
- Assessing Side Effects
- Evaluating Treatment Efficacy
- Alternatives to Premarin for Hormonal Replacement Therapy
- Estrogen Alternatives
- Non-Hormonal Options
Premarin Prescription: A Comprehensive Guide
Consult with your healthcare provider for individual assessment before starting a Premarin prescription. This medication contains conjugated estrogens, primarily sourced from the urine of pregnant mares, and is indicated for hormone replacement therapy in postmenopausal women. Premarin alleviates symptoms such as hot flashes, vaginal dryness, and helps prevent osteoporosis.
Review your medical history with your doctor as certain conditions may contraindicate the use of Premarin. These include a history of breast cancer, blood clots, or liver problems. Monitor for potential side effects like nausea, headache, or breast tenderness, and report severe reactions immediately. Regular follow-ups ensure that the therapy remains safe and effective.
Determine the appropriate dosage as prescribed by your physician. Typically, doctors start with a low dose, gradually adjusting based on symptom relief and side effects. It’s advisable to take the medication at the same time each day to maintain consistent hormone levels in your body.
Inform your provider about any other medications or supplements you are taking, as interactions can occur. Be cautious with herbal products, specifically those containing phytoestrogens, since they may intensify Premarin’s effects or interfere with its efficacy.
Consider lifestyle changes that enhance the benefits of Premarin. Incorporate a balanced diet rich in calcium and vitamin D, engage in regular weight-bearing exercises, and avoid smoking and excessive alcohol consumption to support bone health.
Continuous evaluation of treatment’s necessity is crucial. If symptoms improve, your doctor may advise tapering off the medication. Always follow your healthcare professional’s guidelines regarding medication adjustments.
Understanding Premarin: What It Is and How It Works
Premarin is a medication made from conjugated estrogens, primarily used for hormone replacement therapy in women undergoing menopause. It alleviates symptoms like hot flashes, vaginal dryness, and mood swings by replenishing estrogen levels in the body.
This medication comes in various forms, including tablets and vaginal creams, allowing for flexibility in administration based on patient needs. It is also important to note that Premarin may be prescribed for other conditions such as osteoporosis prevention and certain hormone-related cancers.
The primary mechanism of action involves binding to estrogen receptors in the body. This interaction helps to regulate various physiological functions, including menstrual cycles and bone density. By replacing lost hormones, Premarin promotes stability in hormonal levels, offering relief from menopausal symptoms.
When considering Premarin, discussing potential benefits and risks with a healthcare provider is crucial. Some women may experience side effects, including nausea, headache, and breast tenderness. Regular monitoring and follow-ups ensure that any adverse effects can be addressed promptly.
| Benefit | Possible Side Effects |
|---|---|
| Reduces hot flashes | Nausea |
| Improves vaginal dryness | Headaches |
| Raises mood stability | Breast tenderness |
| Offers bone protection | Weight gain |
Patients should review their medical history, including any history of blood clots, stroke, or certain cancers, as these conditions may influence the suitability of Premarin. This medication highlights the importance of a tailored approach to hormone therapy, ensuring that each patient receives care best suited for her health journey.
Regular communication with a healthcare provider helps to adjust dosages as necessary, optimizing the treatment plan. With thoughtful management, Premarin can significantly enhance the quality of life during the menopausal transition.
Indications for Prescribing Premarin in Hormone Therapy
Premarin is commonly prescribed for the management of menopausal symptoms, such as hot flashes, night sweats, and vaginal dryness. Its estrogen content effectively alleviates these distressing symptoms, improving the quality of life for many women during this transition.
This medication is also indicated for preventing osteoporosis in postmenopausal women, particularly those at high risk due to family history or other factors. Estrogen helps maintain bone density, reducing the incidence of fractures.
In cases of primary ovarian insufficiency or premature menopause, Premarin can replace the hormone deficiency, aiding in the natural hormonal balance and supporting overall health.
Women with specific conditions, such as hormone receptor-positive breast cancer, may require Premarin under a healthcare provider’s guidance for particular management strategies, especially when addressing treatment complications.
Premarin may also alleviate the symptoms associated with certain conditions like endometriosis, providing relief from pain and discomfort during hormonal fluctuations.
Monitoring and regular consultations with a healthcare professional ensure that the benefits of Premarin outweigh any potential risks, tailoring the therapy to each individual’s needs.
Dosage Guidelines for Effective Use of Premarin
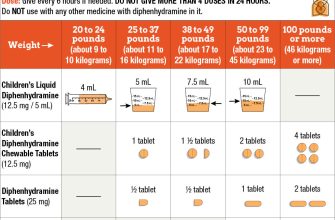
Begin with 0.3 mg of Premarin daily. Adjustments may occur based on individual response and specific medical conditions.
Follow these key points for dosage management:
- Starting Dose: Initiate treatment with 0.3 mg once daily.
- Incremental Adjustments: If necessary, increase dosage gradually, typically no more than 0.3 mg every 3 to 6 weeks.
- Maximum Dose: Commonly, the maximum dosage does not exceed 1.25 mg daily.
Monitor for symptoms and side effects closely. If unwanted effects occur, communicate with your healthcare provider to discuss potential dose modifications.
Always take Premarin at the same time each day to establish a routine. Consistency helps maintain stable hormone levels in the body.
Special populations, such as elderly patients, may require more cautious dosing. Consider renal and liver function when determining the appropriate dose.
Review the necessity of continued therapy with a healthcare provider regularly, especially after the initial treatment phase.
Store Premarin at room temperature, away from moisture and heat. Safeguarding the medication ensures its potency throughout the treatment duration.
Track your experience with the medication. Report any significant changes or concerns to your healthcare provider for timely adjustments.
Potential Side Effects and Risks Associated with Premarin
Monitoring your body’s response during Premarin treatment is critical. Be aware of the following potential side effects:
- Common Symptoms:
- Headaches
- Nausea or vomiting
- Bloating or abdominal pain
- Breast tenderness
- Changes in weight
- Serious Risks:
- Increased risk of blood clots, especially in the legs (deep vein thrombosis) or lungs (pulmonary embolism)
- Higher chance of stroke
- Potential for uterine cancer in women with an intact uterus
- Risk of heart attacks
- Allergic Reactions:
- Skin rash, itching, or hives
- Swelling of the face, throat, or tongue
Consult your healthcare provider immediately if you experience any of these symptoms:
- Sudden headaches or vision changes
- Severe abdominal pain or swelling
- Chest pain or shortness of breath
- Sudden confusion or imbalance
Discuss your family history of cardiovascular disease, hormone-sensitive cancers, or clotting disorders with your doctor before starting Premarin. Tailoring the treatment plan based on individual risk factors enhances safety. Regular follow-up appointments help track any changes in health status.
Consider lifestyle modifications to mitigate risks, such as maintaining a healthy weight, exercising regularly, and avoiding smoking. Your proactive approach contributes to better management of any potential side effects during treatment.
Important Drug Interactions to Consider with Premarin
Consult with your healthcare provider about drug interactions when taking Premarin. Certain medications can affect the levels and efficacy of Premarin, leading to potential complications. Pay close attention to the following interactions:
Anticoagulants and Antiplatelet Drugs
Premarin can enhance the effects of anticoagulants such as warfarin, increasing the risk of bleeding. Regular monitoring of blood clotting times (INR) is recommended when starting or adjusting Premarin dosage.
Anticonvulsants and Barbiturates
Medications like phenytoin and phenobarbital may reduce the effectiveness of Premarin by increasing its metabolism. Your healthcare provider may require dosage adjustments if you are using these medications concurrently.
Always inform your doctor about all medications you take, including over-the-counter drugs and herbal supplements, to ensure safe and effective use of Premarin.
Patient Monitoring and Follow-Up During Premarin Therapy
Regular monitoring during Premarin therapy is crucial to ensure patient safety and treatment effectiveness. Schedule follow-up appointments every three to six months to assess symptoms and side effects. Evaluate hormone levels and adjust dosages as necessary based on clinical response.
Assessing Side Effects
Monitor for common side effects such as headaches, nausea, or breast tenderness. Encourage patients to report any unusual symptoms immediately. Conduct regular blood pressure checks, as Premarin may influence cardiovascular health. Annual mammograms and gynecological exams are recommended for women on long-term therapy.
Evaluating Treatment Efficacy
Assess the effectiveness of therapy by discussing symptom relief, especially in menopausal symptoms like hot flashes and vaginal dryness. Document baseline measurements and compare them to current reports. This approach aids in determining if the treatment remains beneficial.
Educate patients about the importance of adherence to therapy. Encourage them to maintain a symptom diary to help track changes and share relevant information during appointments. Adjust therapy as needed based on comprehensive assessments and patient feedback.
Alternatives to Premarin for Hormonal Replacement Therapy
Consider using bioidentical hormone therapy as an alternative to Premarin. These hormones mimic the body’s natural hormones and can be tailored to individual needs. Often derived from plant sources, bioidentical hormones are available in various forms such as creams, gels, and pills, providing flexibility in administration.
Estrogen Alternatives
Estrogen patches and rings, like the Estradiol patch or NuvaRing, deliver hormones directly into the bloodstream, minimizing side effects associated with oral medications. These options often result in stable hormone levels and a reduced risk of blood clots compared to some oral forms.
Non-Hormonal Options
For those who prefer not to use hormones, products like selective serotonin reuptake inhibitors (SSRIs) or gabapentin can alleviate hot flashes and mood swings. Phytoestrogens, found in soy products and red clover, also provide plant-based support for managing symptoms. Each alternative comes with its own set of benefits and considerations; consulting a healthcare provider ensures the best choice tailored to individual health needs.