For those seeking effective solutions for certain infections, the combination of spiramycine and metronidazole presents a promising approach. This pairing harnesses the unique properties of both medications, targeting various bacterial and parasitic infections with precision.
Spiramycine acts primarily against gram-positive bacteria and demonstrates efficacy in treating infections such as toxoplasmosis. It is particularly beneficial for patients who require an alternative to conventional antibiotics. Meanwhile, metronidazole excels at combating anaerobic bacteria and protozoa, making it invaluable for treating conditions like bacterial vaginosis and certain gastrointestinal infections.
The synergistic effect of spiramycine alongside metronidazole enhances their ability to address complex infections. This combination allows for broader coverage and minimizes the risk of developing antibiotic resistance. Healthcare providers often recommend this duo for specific cases, emphasizing the importance of a tailored treatment plan based on individual patient needs.
By understanding how spiramycine and metronidazole work together, individuals can make informed decisions regarding their treatment options. Discussing this combination therapy with a healthcare professional can uncover the most effective strategies for managing infections.
- Spiramycine Metronidazole: An Overview
- Mechanism of Action
- Dosage and Administration
- Understanding Spiramycine: Mechanism of Action
- Metronidazole: Therapeutic Uses and Benefits
- Combined Use of Spiramycine and Metronidazole
- Indications for Spiramycine and Metronidazole Therapy
- Dosage Guidelines for Spiramycine and Metronidazole
- Potential Side Effects and Adverse Reactions
- Contraindications and Drug Interactions
- Patient Management and Monitoring During Treatment
- Future Directions in Spiramycine and Metronidazole Research
Spiramycine Metronidazole: An Overview
Spiramycine combined with metronidazole is a potent treatment option for specific bacterial infections, particularly those caused by anaerobic bacteria. This combination effectively targets infections such as bacterial vaginosis and certain oral infections. Always consult a healthcare provider to determine the appropriateness of this treatment for individual cases.
Mechanism of Action
Spiramycine is a macrolide antibiotic that inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit. Metronidazole, an antiprotozoal and antibacterial agent, disrupts DNA synthesis in susceptible organisms. Together, these drugs enhance therapeutic effectiveness by attacking different aspects of bacterial metabolism.
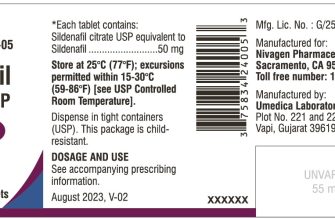
Dosage and Administration
Dosage often depends on the specific infection being treated. Typically, spiramycin is administered in doses of 1 to 3 million units daily, divided into several doses, while metronidazole may be prescribed at 500 mg two to three times daily for 7 days. Adjustments may be necessary for patients with liver impairment or those on other medications. Adhere to the prescribed regimen to ensure optimal results.
Understanding Spiramycine: Mechanism of Action
Spiramycine primarily targets bacterial RNA synthesis, leading to the inhibition of protein production. It selectively binds to the 50S ribosomal subunit, disrupting the peptidyl transferase activity, which ultimately prevents the growth of bacteria.
This antibiotic exhibits a broad spectrum of activity, particularly against Gram-positive bacteria and certain protozoa. Spiramycine is especially effective against organisms such as Streptococcus spp. and Mycoplasma spp., making it a valuable option for treating infections caused by these pathogens.
Spiramycine’s safety profile is generally favorable, leading to its use in various populations, including pregnant women. Its bacteriostatic action allows for effective treatment without leading to resistance as rapidly as some bactericidal agents do.
| Action | Effect |
|---|---|
| Inhibition of RNA synthesis | Prevents protein production |
| Binding to ribosomal subunit | Disruption of bacterial growth |
| Bacteriostatic activity | Reduces risk of resistance |
For optimal therapeutic results, healthcare providers often recommend Spiramycine in combination with other antibiotics, ensuring a comprehensive approach to treatment. Monitoring for potential side effects, though rare, is essential for safe administration.
Metronidazole: Therapeutic Uses and Benefits
Metronidazole is an antibiotic primarily effective against anaerobic bacteria and certain parasites. It stands out in the treatment of various infections, making it a versatile option for healthcare providers.
Primarily, metronidazole treats bacterial vaginosis, a common vaginal infection caused by an imbalance of bacteria. Patients typically respond favorably to the standard oral or topical metronidazole regimens.
The drug is also crucial in managing peptic ulcer disease. It effectively eradicates Helicobacter pylori when used in combination therapy, enhancing healing and preventing recurrence.
In cases of gastrointestinal infections, such as amoebic dysentery and giardiasis, metronidazole acts swiftly to eliminate the causative organisms, offering rapid relief from symptoms.
In surgical settings, metronidazole serves as a prophylactic antibiotic to prevent postoperative infections, especially in surgeries involving the gastrointestinal tract. Its broad spectrum ensures coverage against potential pathogens.
| Indication | Dosage Forms | Typical Dosage |
|---|---|---|
| Bacterial Vaginosis | Oral, Topical | 500 mg twice daily for 7 days |
| Helicobacter Pylori Eradication | Oral | 500 mg twice daily with other antibiotics |
| Amoebic Dysentery | Oral | 750 mg three times daily for 5-10 days |
| Preoperative Prophylaxis | Intravenous | 500 mg before surgery |
Using metronidazole may lead to side effects such as nausea, headache, and a metallic taste in the mouth. Monitoring these effects ensures patient safety and comfort during treatment.
In summary, metronidazole’s broad applications and effectiveness in treating various infections make it a vital tool in modern medicine. Leveraging its benefits can lead to improved patient outcomes and satisfaction.
Combined Use of Spiramycine and Metronidazole
The simultaneous administration of spiramycine and metronidazole can enhance therapeutic outcomes in certain infections. Spiramycine, a macrolide antibiotic, exhibits activity against a range of bacteria, particularly for respiratory and dental infections. Metronidazole, an antiprotozoal and antibiotic, targets anaerobic bacteria and protozoa, making this combination particularly effective in mixed infections.
Healthcare providers often prescribe this combination for treating periodontitis and other polymicrobial infections. The synergistic effect obtained boosts antibacterial activity, leading to improved recovery rates and reduced treatment duration. Regular monitoring of patient response and potential side effects remains essential when utilizing this combination.
Consider dose adjustment based on individual patient conditions and existing polypharmacy to mitigate adverse reactions. Always ensure adequate hydration and discuss the potential for gastrointestinal upset, a common side effect of metronidazole. Encourage adherence to the prescribed regimen to maximize therapeutic success.
This pairing demonstrates promise in off-label uses as well, such as in certain dermatological conditions caused by anaerobic bacteria. Collaboration with a healthcare team is critical for evaluating the appropriateness of this treatment strategy based on clinical presentation.
Indications for Spiramycine and Metronidazole Therapy
Spiramycine is primarily used to treat infections caused by certain bacteria and parasites, particularly in cases of toxoplasmosis during pregnancy. Its application helps prevent the transmission of the parasite to the fetus. Additionally, spiramycin can be used for treating respiratory tract infections and oral infections due to its effectiveness against oral pathogens.
Metronidazole is renowned for its action against anaerobic bacteria and certain protozoa. It’s commonly indicated for conditions such as bacterial vaginosis, intestinal infections, and abdominal infections. Patients often benefit from metronidazole in cases of Clostridium difficile infections, as it effectively targets this challenging bacterium.
Combining spiramycin and metronidazole may serve to enhance treatment in cases of mixed infections where both aerobic and anaerobic bacteria are present. This synergy can lead to improved outcomes in complex infections, especially those involving the gastrointestinal and reproductive tracts.
Both antibiotics are contraindicated in patients with known hypersensitivity to their components. Close monitoring is essential when prescribing these medications, particularly in pregnant individuals and those with liver impairment.
In summary, utilize spiramycin and metronidazole for targeted therapy in specified bacterial and protozoal infections. Tailor treatment approaches based on the specific infection type and patient characteristics for the best results.
Dosage Guidelines for Spiramycine and Metronidazole
Spiramycine is typically administered at a dose of 1-2 million IU every 8 hours for adults, especially for the treatment of certain infections like toxoplasmosis. For children, the dosage varies based on weight: 50,000-100,000 IU per kg of body weight per day, divided into three doses.
Metronidazole is commonly dosed at 500 mg every 8 hours for moderate to severe infections in adults. For specific conditions, such as bacterial vaginosis, a single dose of 2 grams is recommended. In pediatric patients, the dosage is adjusted to 7.5 mg/kg every 8 hours, ensuring the total does not exceed adult dosing guidelines.
Adjustments may be necessary for individuals with liver impairment. Always monitor patients closely during treatment to identify any potential adverse reactions or allergies. Make sure to complete the full course of therapy as prescribed to achieve optimal results.
Consult with a healthcare provider for personalized recommendations, especially if other medications are being taken or if there are underlying health conditions. Accurate dosing and adherence to guidelines enhance treatment efficacy.
Potential Side Effects and Adverse Reactions
Using Spiramycine and Metronidazole may lead to several side effects. It is crucial to monitor your health and report any unusual symptoms to your healthcare provider promptly.
- Nausea and Vomiting: Some individuals experience gastrointestinal discomfort, including nausea or vomiting. Taking these medications with food may help alleviate this issue.
- Diarrhea: This may occur due to changes in gut flora. Staying hydrated is important. If diarrhea persists, consult your doctor.
- Metallic Taste: Metronidazole can cause a metallic or bitter taste in the mouth. This side effect typically resolves after completing the course of treatment.
- Skin Reactions: Allergic reactions, including rashes or itching, may occur. Discontinuing the medication and seeking medical advice is recommended if this happens.
In rare cases, more severe reactions may occur:
- Neurological Effects: Symptoms such as seizures or peripheral neuropathy may arise. Immediate medical attention is necessary if experiencing such symptoms.
- Blood Disorders: Alterations in blood cell counts can occur, leading to anemia or other blood-related issues. Regular blood tests may be needed to monitor these changes.
- Liver Dysfunction: Monitor for signs of liver problems, such as jaundice or severe fatigue. Your doctor may recommend liver function tests periodically.
Always communicate with your healthcare provider regarding any existing medical conditions or medications you are taking. Adjustments to your treatment plan may minimize side effects while maximizing therapeutic benefits.
Contraindications and Drug Interactions
Spiramycine and Metronidazole should be avoided in certain scenarios. Consider the following contraindications:
- Allergy: Do not use if hypersensitive to spiramycin, metronidazole, or similar compounds.
- First trimester of pregnancy: Both medications are contraindicated during the first trimester due to potential fetal risks.
- CNS disorders: Use with caution in patients with neurological conditions, including epilepsy and those with CNS diseases.
- Alcohol consumption: Avoid metronidazole if consuming alcohol, as this may lead to severe nausea, vomiting, and abdominal pain.
Be aware of potential drug interactions when prescribing these medications:
- CYP450 interactions: Metronidazole may inhibit CYP2C9 enzymes, affecting drugs like warfarin, which could heighten bleeding risk. Monitor INR levels closely.
- Anticoagulants: Increased effect of anticoagulants can occur when metronidazole is used. Regular checks are advised.
- Disulfiram: Concurrent use with disulfiram can lead to confusion and psychotic reactions. Avoid using them together.
- Lithium: Metronidazole may elevate lithium levels, increasing toxicity risks. Close monitoring is necessary.
Regular assessments are key to ensure safe administration of spiramycin and metronidazole, especially regarding concurrent medications and patient health history.
Patient Management and Monitoring During Treatment
Monitor liver function tests regularly during Spiramycine and Metronidazole treatment. This helps to identify any hepatic impairment early. Schedule initial tests before starting therapy, then at 2-week intervals during the first month, and subsequently monthly.
Keep an eye on the patient’s symptoms. Assess for any signs of adverse reactions, especially gastrointestinal disturbances such as nausea or diarrhea. Document these findings to adjust dosage if necessary.
Encourage adequate hydration, as both medications can cause gastrointestinal upset. Advise patients to drink plenty of fluids to prevent dehydration.
Discuss potential drug interactions. Review the patient’s medication list thoroughly. Educate patients about avoiding alcohol during Metronidazole therapy to prevent disulfiram-like reactions.
Assess and address any allergic reactions early. Instruct patients to report any rash, itching, or swelling immediately. Provide a plan for managing these reactions, including possible discontinuation of the medication.
Conduct follow-up appointments to evaluate treatment effectiveness. Use clinical assessments and any pertinent laboratory results. If the patient is not improving, reconsider the treatment strategy.
Maintain open communication. Encourage patients to share any concerns, medications taken, or side effects experienced throughout the treatment. This fosters a better understanding of their condition and ensures more personalized care.
Schedule a final evaluation at the end of the treatment course. This should include a comprehensive assessment of symptoms, side effects, and overall response to therapy. Adjust follow-up care based on findings.
Future Directions in Spiramycine and Metronidazole Research
Research should focus on combination therapy involving spiramycin and metronidazole for enhanced antimicrobial efficacy. Exploring synergistic effects could optimize treatment protocols for polymicrobial infections, particularly those caused by resistant pathogens.
Investigating the pharmacokinetics of spiramycin and metronidazole will provide insights into their metabolism, absorption, and elimination. Detailed studies will help in adjusting dosages for specific patient populations, improving treatment outcomes.
Further exploration into potential anti-inflammatory properties of these drugs can yield new therapeutic approaches for conditions beyond their current applications. Clinical trials assessing the impact of these agents on inflammatory diseases may reveal unexpected benefits.
Utilizing advanced imaging techniques can enhance understanding of how spiramycin and metronidazole affect bacterial biofilms. Future studies may focus on strategies to disrupt biofilm integrity, which is a significant challenge in treating chronic infections.
Exploring alternative delivery methods, such as nanoparticle formulations, can improve the bioavailability and efficacy of spiramycin and metronidazole. This route may enhance patient compliance and therapeutic effectiveness.
Ongoing genomic research should aim to clarify the mechanisms driving resistance to spiramycin and metronidazole. By identifying specific genetic markers, researchers can develop targeted approaches to mitigate resistance development and prolong drug effectiveness.
Collaboration with computational biologists and pharmacologists can facilitate the modeling of drug interactions. These models can predict outcomes in various clinical scenarios and help tailor therapies to individual patient needs.
Education on proper use and potential side effects of spiramycin and metronidazole remains critical. Enhanced training for healthcare professionals will ensure informed decisions regarding treatment options and improve patient safety.
Finally, monitoring long-term outcomes in patients treated with these antibiotics will provide valuable data for evaluating their impact on quality of life and chronic disease management. Continuous assessment will refine future treatment guidelines and enhance patient care.