Yes, acne caused by prednisone can clear up after you stop taking the medication. Corticosteroids like prednisone can lead to skin changes, including increased oil production and inflammation, contributing to breakouts. However, the timeline for resolution can vary. Generally, acne should improve within a few weeks to a couple of months once the body adjusts post-medication.
To facilitate healing, maintain a consistent skincare routine. Opt for non-comedogenic products to avoid clogging pores. Gentle cleansers are your best option to remove excess oil without irritating the skin further. Incorporating salicylic acid or benzoyl peroxide into your regimen may help reduce acne but consult with a dermatologist to tailor the right approach for your skin type.
Stay hydrated and consider a balanced diet rich in antioxidants. Foods like fruits, vegetables, and whole grains can support skin health and recovery. If acne persists beyond a reasonable timeframe, consult a healthcare provider. They might recommend topical treatments or other interventions to address ongoing concerns effectively.
- Will Acne from Prednisone Go Away?
- Managing Acne from Prednisone
- Consulting a Dermatologist
- Understanding Prednisone and Its Side Effects
- How Prednisone Causes Acne: The Mechanism
- The Role of Inflammation
- Managing Acne While on Prednisone
- Duration of Acne Breakouts After Discontinuing Prednisone
- Factors Influencing Acne Persistence from Prednisone
- Effective Treatments for Prednisone-Induced Acne
- Skincare Routine Adjustments During Prednisone Use
- When to Consult a Dermatologist for Severe Acne
- Preventive Measures for Future Acne When Using Prednisone
Will Acne from Prednisone Go Away?
Yes, acne induced by prednisone can improve after you stop taking the medication. The duration and severity of acne vary depending on the individual and the dosage of prednisone. Typically, acne can remain for a few weeks to several months following the discontinuation of treatment. Maintaining a consistent skincare routine can help accelerate the recovery process.
Managing Acne from Prednisone
To help control acne, consider the following strategies:
- Use gentle, non-comedogenic skincare products.
- Keep your skin clean by cleansing twice daily.
- Avoid heavy makeup and skincare that can clog pores.
- Incorporate topical treatments containing benzoyl peroxide or salicylic acid.
Consulting a Dermatologist
If the acne persists or worsens, consulting a dermatologist is advisable. They may prescribe medications or recommend specific treatments tailored to your skin type. Tracking your skin’s response can provide valuable insights into effective strategies.
| Action | Description |
|---|---|
| Skincare Routine | Utilize gentle cleansers and non-comedogenic products. |
| Topical Treatments | Consider benzoyl peroxide or salicylic acid for acne treatment. |
| Consultation | Seek advice from a dermatologist for persistent cases. |
Taking proactive steps can significantly enhance the healing process, providing clearer skin over time.
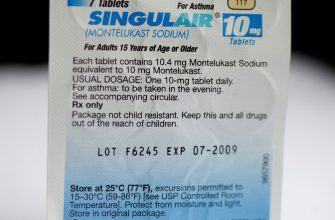
Understanding Prednisone and Its Side Effects
Prednisone is a corticosteroid commonly prescribed to reduce inflammation and suppress the immune system. While effective for various conditions, it can cause side effects, including acne. This skin issue arises due to hormonal changes and increased oil production. It is important to note that acne from prednisone can be persistent, but it often resolves after discontinuing the medication or lowering the dosage.
To manage acne during prednisone treatment, consider the following strategies: maintain a consistent skincare routine with gentle, non-comedogenic products, avoid overly harsh treatments that may irritate the skin, and consult with a dermatologist for tailored advice. Proper hydration and a balanced diet can also support skin health.
Long-term use of prednisone can lead to other skin concerns, such as thinning skin and easy bruising. Monitor your skin’s condition and address concerns with your healthcare provider to adjust your treatment plan if necessary. Regular follow-ups will help track your progress and manage any adverse effects effectively.
Stopping prednisone may lead to a rebound in acne, so transitioning off the medication under medical guidance is recommended. Overall, staying informed and proactive about your skin’s health during prednisone therapy can help minimize issues and promote recovery.
How Prednisone Causes Acne: The Mechanism
Prednisone can lead to acne due to its impact on hormone levels and oil production. This corticosteroid affects the adrenal glands, increasing the secretion of androgens. Elevated androgen levels stimulate sebaceous glands, leading to increased oil production. Excess oil, combined with dead skin cells, clogs pores and creates an environment conducive to acne formation.
The Role of Inflammation
Prednisone also modifies the inflammatory response. While it decreases inflammation overall, it can cause localized skin changes that may exacerbate acne. The alteration in immune response allows for bacteria, like Propionibacterium acnes, to thrive in clogged pores, further aggravating the situation.
Managing Acne While on Prednisone
To manage acne caused by prednisone, consider the following strategies:
- Use non-comedogenic skincare products to avoid clogging pores.
- Keep the skin clean; wash your face twice daily with a gentle cleanser.
- Consider topical treatments with benzoyl peroxide or salicylic acid, which target acne effectively.
- Consult a dermatologist for possible prescription medications if over-the-counter options are ineffective.
- Maintain a balanced diet; reduce intake of sugary and processed foods that can exacerbate acne.
By understanding the mechanism through which prednisone affects the skin, you can take proactive steps to minimize acne flare-ups while receiving necessary treatment.
Duration of Acne Breakouts After Discontinuing Prednisone
Acne breakouts resulting from prednisone can take time to resolve after stopping the medication. Typically, you might experience continued breakouts for
- 1 to 3 weeks
- up to 2 months
- in some cases, even longer
Individual factors influence the duration of acne symptoms. Hormonal fluctuations, skin type, and overall health impact the recovery time.
To help manage breakouts during this period, consider the following recommendations:
- Maintain a gentle skincare routine: Use non-comedogenic products to avoid clogging pores.
- Stay hydrated: Drinking plenty of water supports skin health.
- Monitor your diet: Reducing sugar and dairy may help minimize acne.
- Consult a dermatologist: Professional advice can guide you in choosing suitable treatments for your acne.
Keeping your expectations realistic is key. While the breakouts might persist for a while, a consistent skincare strategy can significantly improve your skin’s condition. Patience and proper care will lead to gradual improvement, and most visible acne should diminish over time.
Factors Influencing Acne Persistence from Prednisone
The duration of acne caused by prednisone often hinges on several key factors. First, the dosage and length of prednisone treatment directly correlate with how long acne may persist. Higher doses or prolonged use can lead to more significant skin changes, making recovery longer.
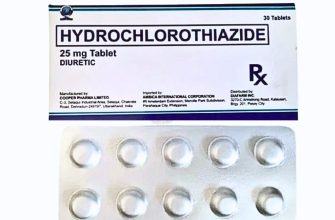
Hormonal fluctuations play a significant role too. Prednisone can increase cortisol levels, which in turn may stimulate oil production in the skin. This can aggravate acne and extend its duration, particularly in individuals prone to hormonal breakouts.
Skin type is another determining factor. Oily skin tends to trap impurities, increasing the likelihood of breakouts persisting after discontinuation of prednisone. Those with sensitive or dry skin may experience a different recovery trajectory.
Post-inflammatory hyperpigmentation can also contribute to the perception of persistent acne. While the bumps may clear up, dark spots can linger, creating the impression that acne is still present. Targeted treatments for hyperpigmentation can be beneficial in these cases.
Additionally, skincare routines impact recovery. Using non-comedogenic products can help minimize the risk of further breakouts, while harsh exfoliants may irritate the skin and delay healing. A gentle approach is advised during the recovery phase.
Lastly, individual health conditions can influence acne persistence. Conditions such as polycystic ovary syndrome (PCOS) or other endocrine disorders may complicate recovery from prednisone-induced acne, requiring tailored treatment approaches.
Effective Treatments for Prednisone-Induced Acne
Over-the-counter topical treatments can significantly reduce prednisone-induced acne. Look for products containing benzoyl peroxide or salicylic acid. These ingredients help unclog pores and reduce inflammation. Apply them directly to affected areas once or twice daily, depending on your skin’s sensitivity.
Incorporate a gentle cleanser into your skincare routine. Choose a non-comedogenic formula that won’t clog pores. Cleansing twice daily can remove excess oil and dirt without irritating the skin.
Consider using an oil-free moisturizer to maintain hydration while preventing breakouts. Opt for lightweight gel-based formulas that hydrate without adding excess oil.
For more severe cases, consult a dermatologist. They may prescribe topical retinoids, which promote cell turnover and can effectively treat acne. In some instances, oral antibiotics might be considered to tackle bacterial growth.
Maintain a balanced diet rich in fruits, vegetables, and whole grains. Staying hydrated and limiting dairy and high-glycemic foods may help minimize acne flare-ups.
Managing stress through mindfulness or regular exercise can also contribute to clearer skin. Elevated stress levels can worsen acne, so techniques like yoga or meditation may offer additional benefits.
Sun exposure can improve acne symptoms in the short term; however, excessive sun can lead to skin damage. Always use a non-comedogenic sunscreen to protect your skin without worsening acne.
Regularly changing pillowcases and towels can help prevent the buildup of bacteria. Proper hygiene practices significantly reduce the risk of acne exacerbation.
Lastly, be patient. Acne from prednisone can take time to clear. Consistency in your skincare routine and treatments is key to seeing improvement.
Skincare Routine Adjustments During Prednisone Use
Use a gentle cleanser specifically formulated for sensitive skin. Look for products without fragrance and harsh chemicals to avoid exacerbating irritation.
Incorporate a lightweight, non-comedogenic moisturizer. This helps maintain hydration without clogging pores. Ingredients like hyaluronic acid or glycerin work well to attract moisture.
Consider adding a salicylic acid-based treatment to address breakouts. Apply it sparingly on affected areas, as it can aid in unclogging pores and reducing inflammation.
Limit exfoliation to once a week. Choose mild exfoliants to prevent over-drying and irritation, which can worsen skin texture during prednisone treatment.
Don’t forget sunscreen. Use a broad-spectrum SPF 30 or higher daily, as prednisone can heighten skin sensitivity to UV rays. Look for physical (mineral) sunscreens containing zinc oxide or titanium dioxide for less irritation.
Evaluate your makeup products; select non-comedogenic options to minimize the risk of clogged pores. Avoid heavy formulations that can exacerbate acne.
Stay hydrated by drinking plenty of water. This simple step supports overall skin health and helps manage dryness associated with prednisone.
Keep an eye on changes in your skin’s response to products. Gradually introduce new items into your routine and discontinue any that cause irritation or worsen breakouts.
Consult with a dermatologist for personalized recommendations if breakouts persist or worsen. They can provide targeted advice tailored to your skin type and treatment plan.
When to Consult a Dermatologist for Severe Acne
Seek a dermatologist if you experience severe acne that persists despite over-the-counter treatments. If your acne leads to emotional distress or significantly affects your quality of life, professional help is warranted.
If acne lesions become painful, inflamed, or form cysts, it’s time to consult a specialist. These signs can indicate a more severe type of acne that may require prescription medications like topical retinoids or oral antibiotics.
When acne scars begin to appear, consult a dermatologist promptly. Early intervention may prevent further skin damage and reduce the risk of scarring. A dermatologist can recommend treatments to minimize scars and improve skin texture.
Consider a visit if you notice unusual skin reactions, excessive redness, or irritation from products. A professional can help identify the cause and suggest alternative treatment options that suit your skin type.
If hormonal changes trigger your acne–common during menstruation or hormonal therapy–professional guidance can help. Dermatologists can prescribe treatments targeting hormonal fluctuations, improving skin condition over time.
Lastly, if you find yourself resorting to multiple products without success, avoid the trial-and-error approach. A dermatologist will analyze your skin and craft a tailored treatment plan, streamlining your journey to clearer skin.
Preventive Measures for Future Acne When Using Prednisone
Maintain a consistent skincare routine. Use gentle cleansers suitable for acne-prone skin to remove excess oil and impurities without causing irritation. Look for non-comedogenic products that won’t clog pores.
Incorporate salicylic acid or benzoyl peroxide into your regimen. These active ingredients help to prevent breakouts by exfoliating the skin and killing bacteria. Start with lower concentrations to assess your skin’s tolerance.
Moisturize regularly with lightweight, oil-free moisturizers. Hydrated skin can better withstand the effects of prednisone and reduce the likelihood of acne associated with dryness.
Stay hydrated. Drinking plenty of water helps maintain skin health and may reduce the risk of breakouts. Aim for at least eight glasses daily.
Pay attention to your diet. Reduce sugar and refined carbohydrates, which can trigger acne flare-ups. Focus on whole foods, including fruits, vegetables, lean proteins, and healthy fats.
Limit touching your face. Frequent contact transfers oils and bacteria, increasing the likelihood of breakouts. Maintain cleanliness by washing your hands regularly.
Keep hair products away from your face. Hair gels, oils, or sprays can contribute to clogged pores. Tie back hair or switch to formulas that are non-comedogenic.
Consult with your healthcare provider for additional options. They may recommend topical treatments or adjustments in your prednisone dosage that can help minimize acne risks.